Overview
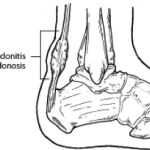 An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).
An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).
Causes
There are a number of factors that can increase the risk of an Achilles tendon rupture, which include the following. Youre most likely to rupture your Achilles tendon during sports that involve bursts of jumping, pivoting and running, such as football or tennis. Your Achilles tendon becomes less flexible and less able to absorb repeated stresses, for example of running, as you get older. Small tears can develop in the fibres of the tendon and it may eventually completely tear. There is a very small risk of an Achilles tendon rupture if you have Achilles tendinopathy (also called Achilles tendinitis). This is where your tendon breaks down, which causes pain and stiffness in your Achilles tendon, both when you exercise and afterwards. If you take quinolone antibiotics and corticosteroid medicines, it can increase your risk of an Achilles tendon injury, particularly if you take them together. The exact reasons for this aren't fully understood at present.
Symptoms
The classic sign of an Achilles' tendon rupture is a short sharp pain in the Achilles' area, which is sometimes accompanied by a snapping sound as the tendon ruptures. The pain usually subsides relatively quickly into an aching sensation. Other signs that are likely to be present subsequent to a rupture are the inability to stand on tiptoe, inability to push the foot off the ground properly resulting in a flat footed walk. With complete tears it may be possible to feel the two ends of tendon where it has snapped, however swelling to the area may mean this is impossible.
Diagnosis
In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests.
Non Surgical Treatment
Two treatment options are casting or surgery. If an Achilles tendon rupture is untreated then it may not heal properly and could lead to loss of strength. Decisions about treatment options should be made on an individual basis. Non-surgical management traditionally is selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery. The goal of casting is to allow the tendon to slowly heal over time. The foot and ankle are positioned to bring the torn ends of the tendon close together. Casting or bracing for up to 12 weeks or more may be necessary. This method can be effective and avoids some risks, such as infection, associated with surgery. However, the likelihood of re-rupture may be higher with a non-surgical approach and recovery can take longer.
Surgical Treatment
The surgical repair of an acute or chronic rupture of the Achilles tendon typically occurs in an outpatient setting. This means the patient has surgery and goes home the same day. Numbing medicine is often placed into the leg around the nerves to help decrease pain after surgery. This is called a nerve block. Patients are then put to sleep and placed in a position that allows the surgeon access to the ruptured tendon. Repair of an acute rupture often takes somewhere between 30 minutes and one hour. Repair of a chronic rupture can take longer depending on the steps needed to fix the tendon.
Prevention
Achilles tendon rupture can be prevented by avoiding chronic injury to the Achilles tendon (i.e. tendonitis), as well as being careful to warm up and stretch properly before physical activity. Additionally, be sure to use properly fitting equipment (e.g. running shoes) and correct training techniques to avoid this problem!
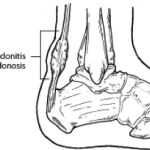 An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).
An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).Causes
There are a number of factors that can increase the risk of an Achilles tendon rupture, which include the following. Youre most likely to rupture your Achilles tendon during sports that involve bursts of jumping, pivoting and running, such as football or tennis. Your Achilles tendon becomes less flexible and less able to absorb repeated stresses, for example of running, as you get older. Small tears can develop in the fibres of the tendon and it may eventually completely tear. There is a very small risk of an Achilles tendon rupture if you have Achilles tendinopathy (also called Achilles tendinitis). This is where your tendon breaks down, which causes pain and stiffness in your Achilles tendon, both when you exercise and afterwards. If you take quinolone antibiotics and corticosteroid medicines, it can increase your risk of an Achilles tendon injury, particularly if you take them together. The exact reasons for this aren't fully understood at present.
Symptoms
The classic sign of an Achilles' tendon rupture is a short sharp pain in the Achilles' area, which is sometimes accompanied by a snapping sound as the tendon ruptures. The pain usually subsides relatively quickly into an aching sensation. Other signs that are likely to be present subsequent to a rupture are the inability to stand on tiptoe, inability to push the foot off the ground properly resulting in a flat footed walk. With complete tears it may be possible to feel the two ends of tendon where it has snapped, however swelling to the area may mean this is impossible.
Diagnosis
In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests.
Non Surgical Treatment
Two treatment options are casting or surgery. If an Achilles tendon rupture is untreated then it may not heal properly and could lead to loss of strength. Decisions about treatment options should be made on an individual basis. Non-surgical management traditionally is selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery. The goal of casting is to allow the tendon to slowly heal over time. The foot and ankle are positioned to bring the torn ends of the tendon close together. Casting or bracing for up to 12 weeks or more may be necessary. This method can be effective and avoids some risks, such as infection, associated with surgery. However, the likelihood of re-rupture may be higher with a non-surgical approach and recovery can take longer.

Surgical Treatment
The surgical repair of an acute or chronic rupture of the Achilles tendon typically occurs in an outpatient setting. This means the patient has surgery and goes home the same day. Numbing medicine is often placed into the leg around the nerves to help decrease pain after surgery. This is called a nerve block. Patients are then put to sleep and placed in a position that allows the surgeon access to the ruptured tendon. Repair of an acute rupture often takes somewhere between 30 minutes and one hour. Repair of a chronic rupture can take longer depending on the steps needed to fix the tendon.
Prevention
Achilles tendon rupture can be prevented by avoiding chronic injury to the Achilles tendon (i.e. tendonitis), as well as being careful to warm up and stretch properly before physical activity. Additionally, be sure to use properly fitting equipment (e.g. running shoes) and correct training techniques to avoid this problem!
